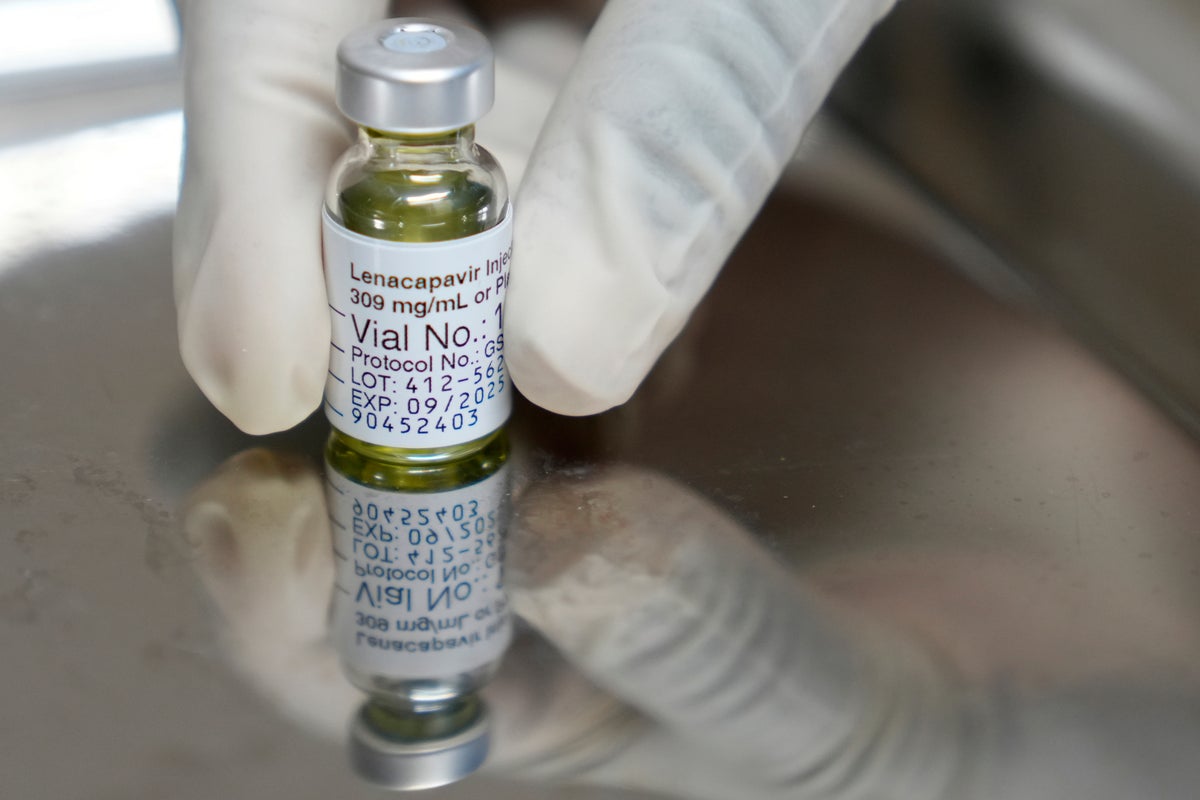
The two pharmaceutical companies are supposed to receive the funding needed to produce HIV Lenacapavir, in what a key researcher has read a big step “to gain pocket”-as an important tool to end HIV/AIDS-to-low-income countries.
Lenacapavir will cost a patient in 120 medium and average countries since 2027 under $ 40 (£ 30) a year.
The distribution of jabs has been questioned after a profound reduction in the costs of global aid, especially by Donald Trump in the United States, and increases fears among HIV researchers that “prevention of a casualties will be”, “preventing a casualties.”
Lenacapavir is a preventive front twice a year that provides almost total protection against virus production. This is described as the closest thing we have to the HIV vaccine.
The Gates Foundation has announced that it has announced plans to prepare budgets to hetero laboratories to prepare a number of initial and guaranteed doses for the Hyderabad -based pharmaceutical company for these doses. This allows it to produce the general version of Lenacapavir faster. The price of a brand made by Gilead is sold for $ 28218.
The Foundation said it has invested more than $ 80 million in the long -term JAB. Most of these go to hetero laboratories.
At the same time, Clinton’s Health Access Initiative, the World Health Organization Initiative and the South African Research Foundation, the Wits Institute of Health and Reproductive Institute and the HIV Institute announced the agreement on the DR Reddy’s Laboratories.
Professor Becker welcomed these partnerships, “obviously,” he added: “Its entry into a more affordable area means that our governments can plan in the future to incorporate it into our response plans.”

“Scientific advances like Lenacapavir can help us end the HIV epidemic – if they are available to people who can get the most out,” said Trevor Mundel, the head of the World Health Foundation. “We are committed to ensuring that people with the most danger, who can handle it, do not go behind.”
These cheaper doses will be available to more than 100 countries. However, according to Beatriz Grinsztejn, president of the International AIDS Association (IAS), nations throughout Latin America, who have high HIV loads and participated in Lenacapavir trials – for example Brazil – do not lose access to cheaper doses.
Last December, an agreement between Gilad and World Investors – led by the US President’s Emergency Program for AIDS and the World Fund for AIDS, TB and malaria – was carried out to provide sufficient doses of LernophaoPavir to protect at least two million people over three years.
Gilad said the doses do not make a profit, but it did not make the price public. And countries are still forced to find money in their growing budgets to pay for their costs.
At the same time, six pharmaceutical companies, including Hetro and Dr. Redi, were licensed by Gilead to produce public versions of Jab, designed to reduce prices in the long run. While the Gilead deal allows public manufacturers to produce Lenacapavir, new transactions with the Gates Foundation and others are designed to provide funding and incentives to be financially suitable for manufacturers to produce the risk of producing higher doses in a shorter period of time. The first general doses under this transaction are forecast around the end of 2027.

Despite the Trump administration’s reduction in overseas costs, which initially questioned Pepfar’s role in securing Lenacapavir, the State Department announced on September 4 that it would go with its contribution to two million people with JAB by 2028.
“The United States is an example of Rubio’s Foreign Minister in the first program of life in life,” said Jeremy Levin, a senior foreign aid, humanitarian affairs and religious freedom. “This innovation makes America champion, the government’s goal of ending mother -to -HIV child transfer in the second term of President Trump and serves as an important catalyst for more investment in the world and private sector to access these pioneering drugs.”
Professor Becker said he recently feels “promising” that trades are seeing, “more access and so influence because this is what we need. We need this innovation to be on a scale in all areas where the virus is circulating so that it can fulfill its potential.”
However, despite PEPFar’s commitment to finance the Lenacapavir production funding, the US withdrawal from financing the widespread prevention services could be compromised.
He explained that groups that can benefit from Lenacapavir include some people who, because of laws that punish gay relationships, find the sale of sex and drugs hard to find the most difficult access to health care.
“There is still work on desigmatism services, making services friendly, and making services available,” he said.
“They had these drops, they had community -based services, non -governmental services, peer services, so they have to be replaced quickly to ensure that now we have access to the product, we have someone who can really … [it]”
Without personnel and infrastructure to deliver Lenacapavir, even if enough doses are done, it will not reach the people who need it.
“We welcome Lenacapavir genes who are affordable – a fundamental step in expanding access,” said IAs. “But availability in 2027 is still very out of the question. With HIV’s response to the budget crisis, countries are currently doing difficult trade,” he said.
This story is part of The Independent Revision of global aid Series